Exploring the Path to a Medical Career: Training and Opportunities
Understanding the Foundations of Medical Training
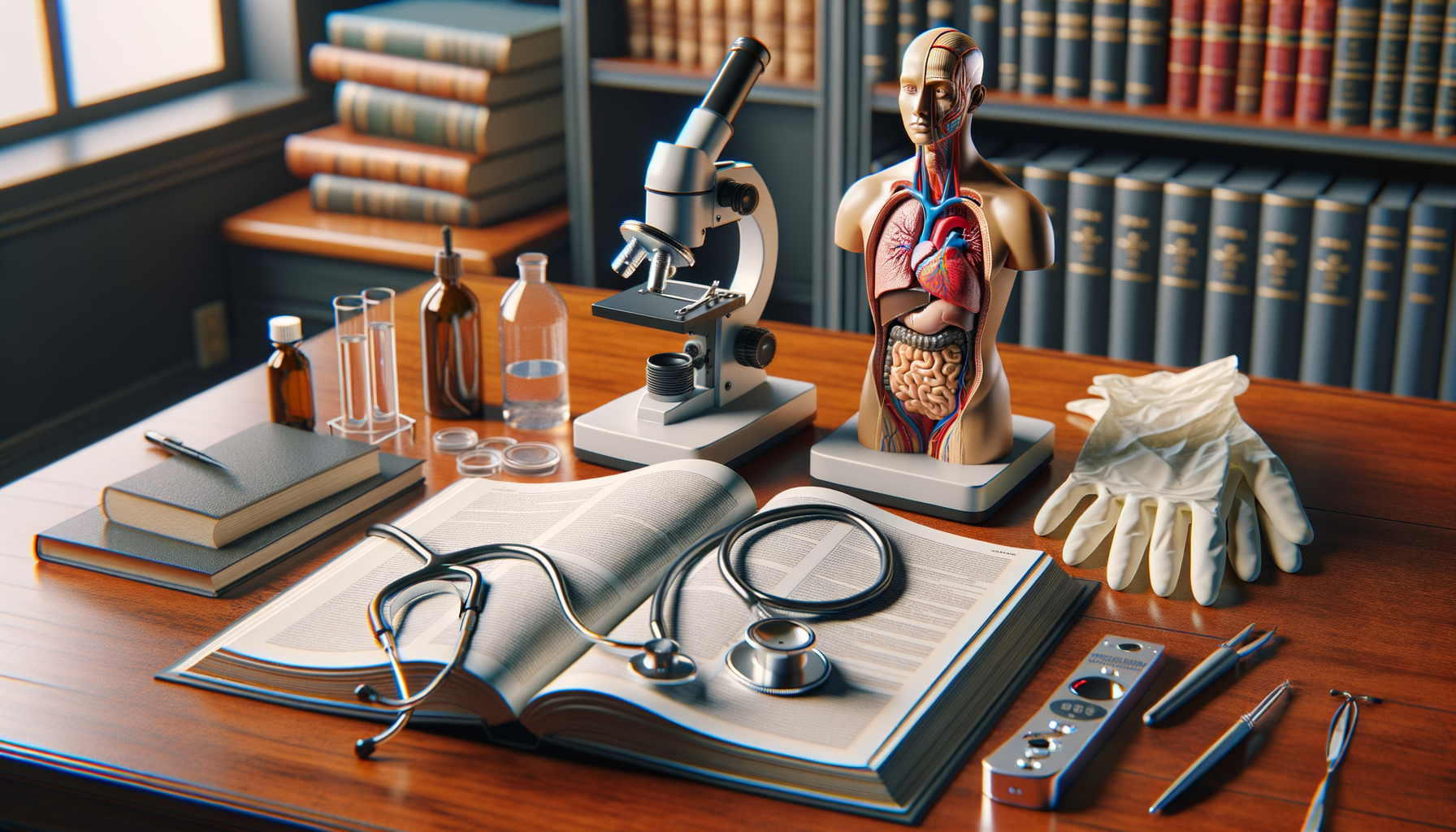
Medical training is an intricate and demanding process that serves as the backbone of healthcare systems worldwide. It is designed to equip aspiring healthcare professionals with the necessary skills, knowledge, and attitudes required to provide high-quality care. The journey begins with a solid foundation in basic sciences, such as anatomy, physiology, and biochemistry, which are essential for understanding the human body and its functions.
In addition to the scientific aspects, medical training also emphasizes the development of clinical skills. Students engage in hands-on experiences through clinical rotations, where they are exposed to real-life medical scenarios under the supervision of experienced practitioners. This practical approach helps them apply theoretical knowledge to patient care, fostering critical thinking and problem-solving abilities.
Moreover, medical training is not solely about acquiring technical skills. It also focuses on cultivating empathy, communication, and ethical decision-making. These soft skills are vital for building strong patient-doctor relationships and ensuring patient-centered care. By integrating these elements, medical training aims to produce well-rounded professionals who can adapt to the dynamic nature of healthcare.
Challenges and Innovations in Medical Education
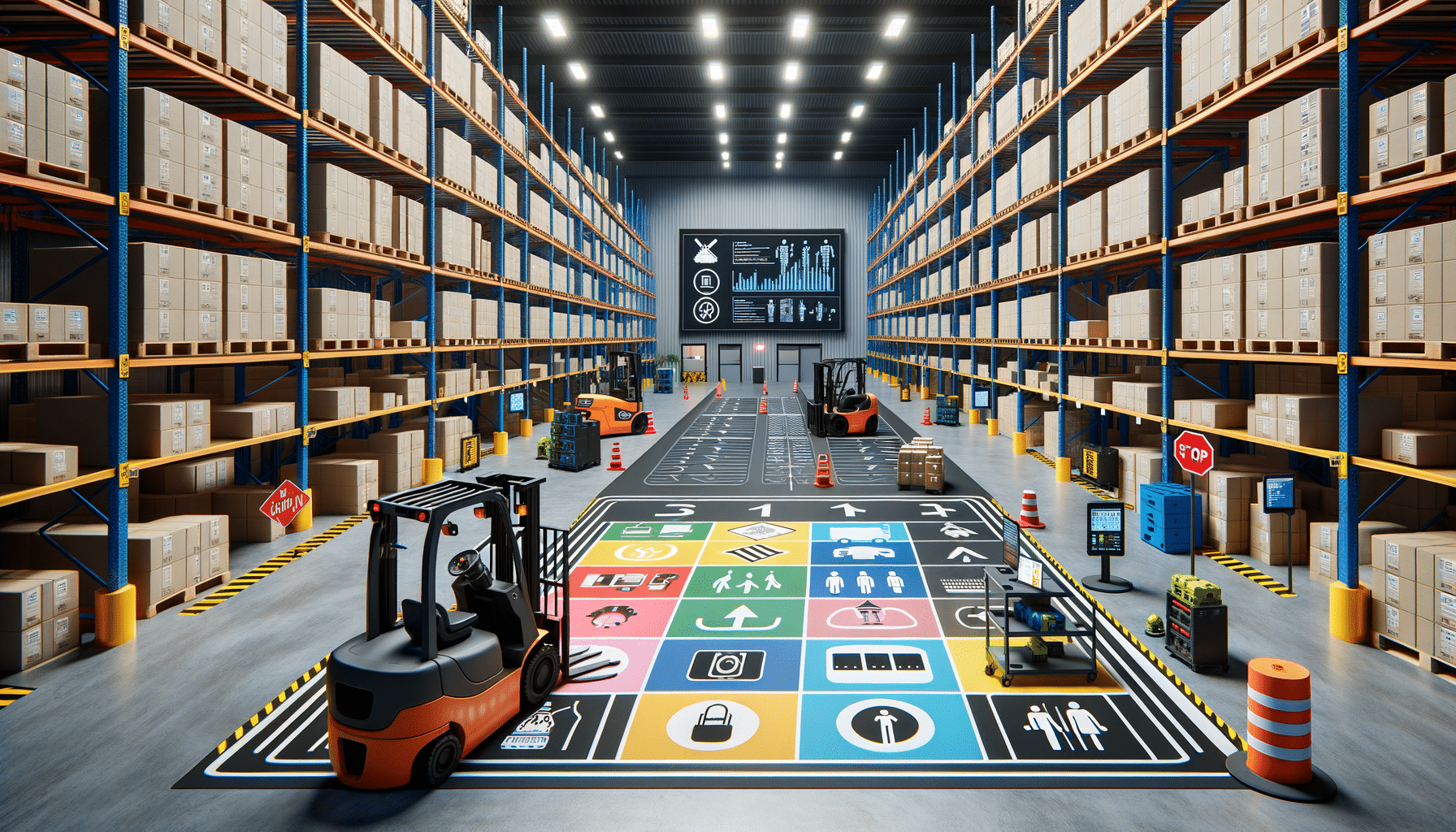
The field of medical education is constantly evolving to address the challenges posed by advancements in technology, changing patient demographics, and emerging global health issues. One of the significant challenges is the need to incorporate new technologies into the training process. Simulation-based education, for instance, has become a cornerstone of modern medical training, allowing students to practice procedures in a risk-free environment.
Another challenge is ensuring that medical curricula remain relevant and comprehensive. As medical knowledge expands, educators must continuously update and refine course content to include the latest research findings and treatment modalities. This requires collaboration among academic institutions, healthcare organizations, and regulatory bodies to develop standardized curricula that meet the needs of both students and the healthcare system.
Innovation in medical education also extends to teaching methodologies. Problem-based learning (PBL) and team-based learning (TBL) are increasingly being adopted to promote active learning and collaboration among students. These approaches encourage students to take ownership of their learning process, enhancing their ability to work effectively in multidisciplinary teams.
The Role of Continuing Medical Education (CME)
Continuing Medical Education (CME) plays a pivotal role in ensuring that healthcare professionals remain competent and up-to-date with the latest developments in their fields. CME provides opportunities for lifelong learning, allowing practitioners to expand their knowledge, refine their skills, and stay informed about new medical technologies and treatment protocols.
CME activities come in various forms, including conferences, workshops, online courses, and peer-reviewed journals. These platforms offer a wealth of information on diverse topics, ranging from clinical advances to healthcare policy changes. By participating in CME, healthcare professionals can earn credits that contribute to their professional development and licensure requirements.
Moreover, CME fosters a culture of continuous improvement within the medical community. It encourages professionals to critically evaluate their practice, identify areas for enhancement, and implement evidence-based strategies to improve patient outcomes. In this way, CME not only benefits individual practitioners but also contributes to the overall advancement of healthcare quality and safety.